Removal of Adhesions in Uterus
What is the Removal of Adhesion inside Uterus?
Intrauterine adhesions that result in an absence of menses or menstrual cycle after curettage were first described in 1894 by Fritsch. Later in 1950, Asherman described the history cases of 29 women with amenorrhea which was secondary to trauma of the uterine cavity, the Asherman’s syndrome (AS).
When the trauma occurs in the basalis layers of the endometrium, Asherman’s Syndrome occurs after that. AS is a medical condition that indicates the presence of intrauterine adhesions or adhesions in the endocervix. It has a consequent risk of hypomenorrhea/amenorrhea, pregnancy loss, reduced fertility, and abnormal placentation.
Everything You Need to Know About Removal of Adhesion inside Uterus
Asherman’s Syndrome | Common Asherman’s Syndrome | Causes | Test Are Used | How is Treat | Can Be Prevented
What is Asherman’s syndrome?
Asherman’s syndrome (AS) is a rare medical condition, which a patient is not born with. It refers to the formation of scar tissue in the uterus or cervix. Due to these scar tissues, the walls of these organs stick together and reduce the size of the uterus. Asherman’s syndrome is also called intrauterine synechiae or uterine synechiae where Synechiae means adhesions. It is also called intrauterine adhesions (IUA).
How common is Asherman’s syndrome?
Asherman’s syndrome is considered a rare disease as it affects very few women. It is hard to know how many women it affects because it is not always diagnosed. Research estimates that IUA happens in nearly 20% of women who have had dilation and curettage (D&C) after pregnancy complications.
What are the symptoms of Asherman’s syndrome?
The symptoms of AS depend upon different women where some women will see no symptoms and other women will have normal periods. Some of the symptoms are:
- Having light periods (hypomenorrhea)
- Having no periods (amenorrhea)
- Having severe cramping or pain.
- Being unable to get or stay pregnant
Sub Treatments For Fertility Enhancing Surgeries
We are one of the Best IVF Clinic in Delhi NCR!
69K
Subscribers
4.6 (615 reviews)
4.2 (904 reviews)
3.5 (265 reviews)

5 Out Of 5
What causes Asherman’s syndrome?
There are some causes of AS. Some of them are:
- Scar tissue caused by uterine surgery like dilation and curettage (D&C). (This causes over 90% of IUA.)
- Scar tissue after a Cesarean section or from sutures used to stop hemorrhages during normal delivery.
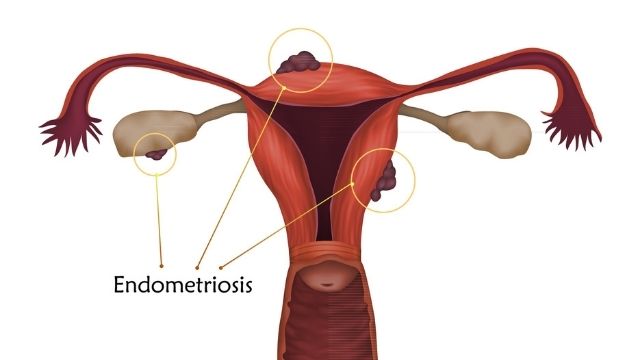
- Endometriosis
- Infections in the reproductive organs
- Radiation treatment
What tests are used to diagnose Asherman’s syndrome?
Your doctor will take your medical history and will do a physical examination. It is to be noted that such Adhesions can not be diagnosed by any physical examination. In this case, a cervical blockage might be indicated if an instrument cannot enter the cervix.
Your doctor might do hormone tests to rule out any endocrine problems, or he or she might use hormones to induce bleeding if you have any menstrual disturbances.
Another option to diagnose Asherman’s syndrome is saline infusion sonography (SIS), also called sonohysterosonography, or ultrasound of the uterus. SIS uses a saline solution that flows into the uterus to make imaging of the uterine cavity clearer even on a 2D scanning.
The best way to diagnose this syndrome is hysteroscopy. During this procedure, the doctor puts a telescopic-camera into the uterus to see the whole uterine cavity. Hysterosalpingography combines an X-ray and radio-opaque material or a dye that is put into the fallopian tubes and the uterus to indicate any growths or blockages. Filling defects in the uterine cavity may suggest intrauterine synechiae.
How is Asherman’s syndrome treated?
The goal of treating this syndrome is to help the uterus regain its normal shape and size. In addition to diagnosis, hysteroscopy is a procedure that can also treat IUA by cutting the adhesions with small scissors, lasers, or other types of instruments that use hooks or electrodes. You might have to have more than one procedure to get the desired results. After the procedure, your doctor may prescribe some hormones to let the uterine lining grow back correctly. This way you will have normal periods again.
Can Asherman’s syndrome be prevented?
According to some researchers, a woman who underwent uterine surgery or injuries to the uterus should also take hormone therapy or go for mechanical separation of uterine walls to prevent IUA. This way a stent is left in the uterus for some time in order to stop the development of intrauterine adhesions. Women who have had uterine surgeries may require imaging tests before trying to get pregnant to see if there are any adhesions.
Some researches have shown that the timing of D&Cs can influence the formation of adhesion. For example, adhesion is more likely to happen if the postpartum D&C is done two to four weeks after the delivery. The uterus that was recently pregnant, can be susceptible to the trauma of the basal layer of the endometrium, which can develop into intrauterine adhesions. An estimation shows that more than 90% of adhesion cases occur after pregnancy-related curettage.
What is the outlook/ prognosis for Asherman’s syndrome?
After the right treatment, when the uterus goes back to its normal shape and size, problems with menstruation will be resolved. This should help a woman to become pregnant if she wants.
Conclusion
In the last 20 years, most women with asherman’s syndrome returned to normal menstruation cycle and there is about 60% percent of women who conceived again.
Patient Guide
Along with treating our patients, we also guide them with the help of our educational blogs and videos.
Educational Blogs
Why do blastocyst not implant?
The reasons for an unsuccessful implantation are very uncommon and rare as well. Blastocyst provides a greater chance of becoming pregnant therefore the procedure is handled properly as well.
What happens after blastocyst transfer?
Before jumping to the immediate question first let’s have a small brief of what is blastocyst transfer. Blastocyst transfer is the transfer of embryos that have achieved a higher stage of development.

Can blastocyst fall out?
Maximum patients worry about what they can do or cannot do after an embryo transfer. They have the fear that if they do something wrong, the embryo would not attach or fall out.
Educational Videos

What is TORCH test in infertility and why is it done?
There are numerous tests that are available to infertile couples that are recommended by some doctors, which might help them determine the cause of their infertility. One such test is the TORCH test.

What is Prolactin Hormone?
Prolactin is a hormone produced by the pituitary gland present at the brain’s base. It is best known for its role in lactation, or milk production, in breastfeeding women.However, Prolactin also plays other important roles in both men and women, such as regulating the immune system, stimulating the growth of new blood vessels, and influencing behaviour and reproductive function. In this blog, we will explore what Prolactin is, how it works, and what happens when there are imbalances in prolactin levels.

Frequently Asked Questions about Low AMH
Primordial and Preantral follicles produce AMH. So the AMH level indicates the number of eggs or egg reserves you have in your ovary. Putting simply, if your AMH level is low, then the number of eggs in your ovary is less.
Frequently Asked Questions
Can obesity or being overweight have an impact on a man’s fertility?
Comprehensive Fertility Treatments | Gynaecology Procedures | Menopause Management | Pregnancy Care | Maternity & Birthing Call +919990044555A short article by IVF experts...
Does testicular temperature have an impact on male fertility
IVF specialists of the best IVF centre in Ghaziabad – Gunjan IVF World share an informative blog on one of the most ignored factors of male infertility. It is an alarming fact to...
Is male menopause a myth or reality ?
IVF specialists of the best IVF centre in Ghaziabad – Gunjan IVF World debunk the myths about male menopause through this informative blog Menopause as a term is extremely common...
Advanced IVF Care with Clinical Excellence